Cryptococcal meningitis
- Cryptococcal infections, including cases of fatal cryptococcal meningitis and disseminated cryptococcal infections have been reported with fingolimod in the postmarketing setting1
- Due to the extent of missing data, the exact pattern of the relationship to duration of treatment remains unclear. The precision of incidence estimates are low due to the small number of cases
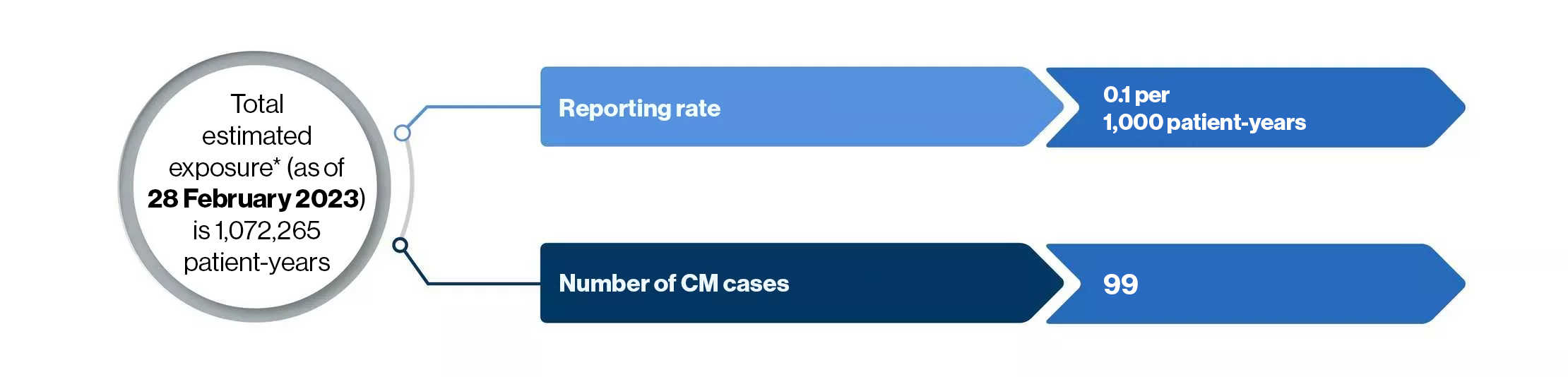
*Total commercial exposure to fingolimod
About CM
About CM
- Cryptococcosis is a pulmonary or disseminated infection acquired by inhalation of soil contaminated with the encapsulated yeast Cryptococcus neoformans or C. gattii2
- After inhalation, Cryptococcus may disseminate, frequently to the brain and meninges, typically manifesting as microscopic multifocal intracerebral lesions2
- CM signs/symptoms result from cerebral edema and include non specific symptoms such as headache, blurred vision, confusion, depression, agitation, other behavioral changes. Except for ocular or facial palsies, focal signs are rare until relatively late in the course2
- CM diagnosis is suggested by symptoms of an indolent infection in immunocompetent patients and a more severe, progressive infection in immunocompromised patients. Unexplained progressive brain dysfunction, particularly in those with depressed cell-mediated immunity2
- Chest x-ray, urine collection, and lumbar puncture are frequently the initial diagnostic tests done
- Elevated CSF protein and a mononuclear cell pleocytosis are usual in cryptococcal meningitis
- The latex test for cryptococcal capsular antigen is positive in CSF or blood specimens or both in > 90% of patients with meningitis and is generally specific
- General recommendations for management of CM
- Amphotericin B, flucytosine, and fluconazole are antifungal medications shown to improve survival in patients with cryptococcal infections2
